發生原因:
ETIOLOGY — Bursitis may result from any one or combination of the following causes:
●Direct injury or trauma.
●Prolonged pressure. This can occur after prolonged kneeling or leaning on an elbow.
●Overuse or strenuous activity.
●Crystal-induced arthropathy. This can be seen with longstanding or tophaceous gout.
●Inflammatory arthritis such as rheumatoid arthritis (RA) or spondyloarthritis.
●Infection (septic bursitis). This can occur due to transcutaneous transit of bacteria from penetrating injury or microtrauma (most commonly) or hematogenous seeding (less commonly). Note that the presence of another cause of bursitis does not exclude the possibility of concurrent infection (eg, superinfection of a tophaceous olecranon bursa).
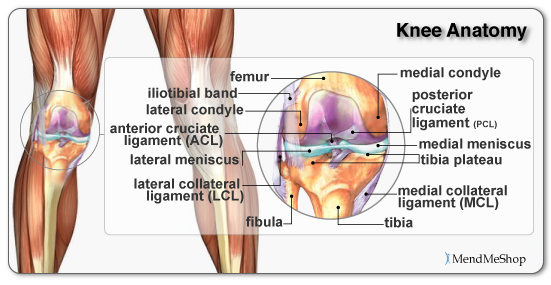
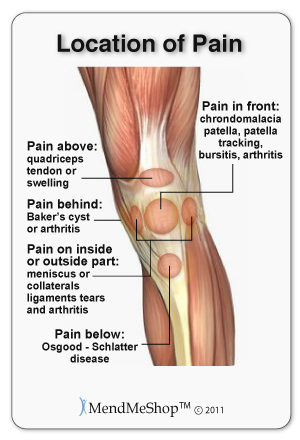
CLINICAL PRESENTATION AND PHYSICAL EXAMINATION — Among patients with bursitis, obvious signs of swelling and inflammation may be evident upon physical exam only in superficial processes, such as olecranon, prepatellar, infrapatellar, or retrocalcaneal bursitis. Common but deeper processes, such as anserine, subacromial, or trochanteric bursitis, are seldom associated with visible swelling or erythema. There are also differences in presentation based on the acuity or chronicity of the underlying disease process.
是否需要影像學檢查?
The need for imaging — Imaging studies are typically not necessary, particularly in the case of superficial bursa where the signs of inflammation are demonstrated on the physical examination. The need for imaging in the evaluation of deep bursal syndromes is dependent on other factors, and a precise anatomical diagnosis is often not necessary, particularly in the initial evaluation. There is little evidence that a strong correlation exists between the clinical presentation of local tenderness and the anatomical evidence (seen on ultrasound or magnetic resonance imaging [MRI]) of inflammation of the deeper bursae [4,5].
However, there are some instances in which imaging is appropriate. We use imaging in the following scenarios:
●Any situation in which the establishment of a more accurate diagnosis seems imperative. As an example, the classical presentation of iliopsoas bursitis is the presence of groin pain, accentuated by flexing the hip against resistance (see 'Iliopsoas bursitis' below). This finding would also be characteristic of labral tears, early avascular necrosis of the femoral head, or any inflammatory process involving the hip joint. All of these syndromes could be associated with a normal plain radiograph of the hip, and making a definitive early diagnosis is warranted. By contrast, the need to establish a definite diagnosis of subacromial bursitis in the shoulder is generally not critical at the time of presentation.
●Conditions in which the entrance of a needle into the area occupied by the bursa is associated with a significant risk of injury to an adjacent neurovascular structure. This is a factor in attempting an aspiration of the iliopsoas bursa related to its proximity to the femoral artery and nerve.
治療:
PRINCIPLES OF MANAGEMENT — With the exception of septic bursitis, the underlying management principle is that isolated bursitis is a self-limited condition that is reversible. In addition, unlike cartilage, the bursa has the ability to heal. In short, bursitis will get better. Therefore, the goal of treatment is to relieve the immediate symptoms, to prevent the secondary complications related to immobilization (muscle atrophy and joint contracture), and to maintain range of motion. Bursitis that is associated with adjacent pathology may improve partially with treatment, but optimal treatment may require techniques specifically directed at the adjacent pathology as well.
Patients should be taught the principles of joint protection and, unless contraindicated, affected individuals should also receive analgesia, which usually consists of a nonsteroidal antiinflammatory drug (NSAID). In addition, our initial approach to the management of presumed inflammation of the deeper bursae is typically an intralesional injection of a combination of local anesthetic and glucocorticoid. However, we do not recommend the use of intralesional glucocorticoids in the treatment of the superficial forms of bursitis (olecranon, prepatellar, and Achilles) due to the risk of infectious complications in the setting of skin atrophy. Application of an ice pack (for no more than 20 minutes at a time) can offer therapeutic relief of a superficially inflamed bursa. For deep forms of bursitis like trochanteric bursitis, a heating pad is often more helpful than ice. Caution must be taken so that a patient does not use the heating pad for more than 20 minutes at a time or fall asleep on the heating pad, as to avoid thermal burn
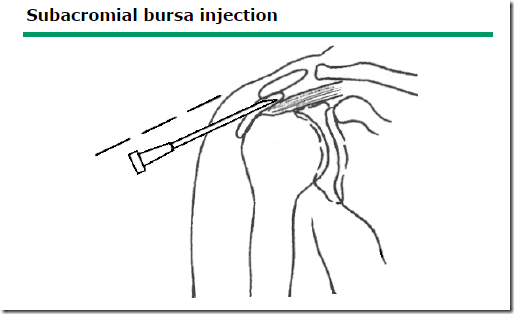
Among patients with presumed inflammation of deep bursae, we suggest that initial therapy include an intralesional injection of a combination of local anesthetic and glucocorticoid . If the original injection provides several weeks of significant relief, the diagnosis of a soft tissue process seems secure, a repeat injection may be tried if symptoms warrant.